Should You Track Calories on a GLP-1 Medication?
Important: This article is for educational purposes only and is not medical advice. Always follow your healthcare provider's guidance about nutrition while taking GLP-1 medications.
If you're taking a GLP-1 medication like semaglutide (Ozempic, Wegovy) or tirzepatide (Mounjaro, Zepbound), you've probably wondered: should I be tracking my calories?
The internet is full of conflicting advice. Some influencers swear that calorie tracking is essential for "maximizing results." Others claim the medication does all the work, so why bother? Your Great Uncle lost 50 pounds without tracking a single thing, but your coworker insists you need to log every bite.
So what does the evidence actually say?
Let's look at what we know about calorie tracking, GLP-1 medications, and whether combining the two makes sense for your specific situation.
What We Know About Calorie Tracking in General
First, let's separate GLP-1 medications from the equation and look at what research tells us about calorie tracking for weight loss in general.
The Evidence Says It Can Work
Multiple studies have shown that people who track their food intake tend to lose more weight than those who don't.
One study following a diabetes prevention program found that consistent tracking predicted an additional seven pounds of weight loss over the course of the program. The key word here is "consistent" - people who tracked regularly did better than those who tracked sporadically.
A meta-analysis looking at digital self-monitoring tools found that about 75% of the time, people who used tracking tools more frequently lost more weight than those who tracked less often.
Research from Duke University showed that people using a free calorie-tracking app achieved meaningful weight loss, with those who were most diligent about tracking (both their food and their weight) losing the most.
So yes, for many people in many contexts, calorie tracking can be an effective tool for weight loss.
But It's Not Magic, and It's Not Universal
Here's what the same research also shows:
Adherence drops off quickly. In one study, participants tracked their food on fewer than 30% of days, even when given apps and support. Most people don't stick with it long-term.
The method matters less than consistency. Whether you use an app, pen and paper, or just increased awareness - what matters most is doing it regularly, not which specific tool you use.
It can backfire for some people. Research on eating disorders found that 75% of people diagnosed with an eating disorder reported using calorie counting tools, and 73% felt it contributed to their disorder. This doesn't mean tracking causes eating disorders, but it does mean that for vulnerable individuals, it can be harmful.
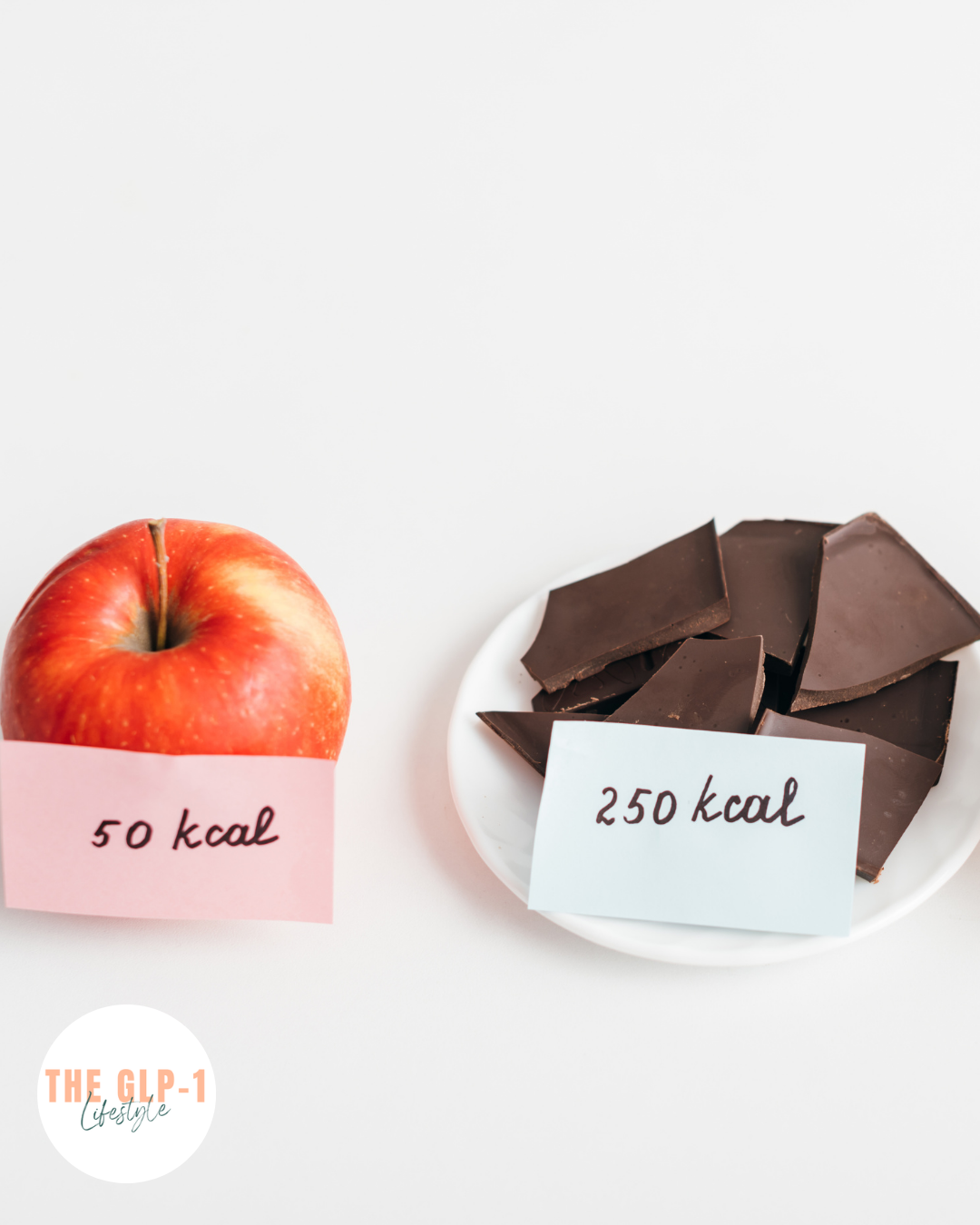
Quality matters more than quantity. A study comparing calorie counting to the USDA's MyPlate approach (focusing on food quality rather than numbers) found similar outcomes. Eating 100 calories of donuts affects your body differently than 100 calories of apples, even though the calorie count is identical.
How GLP-1 Medications Change the Equation
GLP-1 medications work differently than traditional dieting, and that changes the calculus around tracking.
GLP-1 Medications Directly Address the Hunger Problem
Traditional weight loss advice assumes you need to consciously restrict calories through willpower and tracking. But GLP-1 medications work by mimicking a hormone that regulates appetite and food intake at a biological level.
These medications slow gastric emptying (making you feel full longer), reduce cravings, affect brain regions involved in appetite regulation, and can even change how rewarding food feels.
In clinical trials, people taking these medications naturally ate less without being told to count calories or restrict specific foods. The medication was doing the appetite regulation work.
The Results Speak for Themselves - Without Mandatory Tracking
In major clinical trials:
Semaglutide 2.4mg produced an average 14.9% reduction in body weight over 68 weeks
Tirzepatide at 15mg produced an average 20.9% weight loss over 72 weeks
These results were achieved with lifestyle intervention support, but participants weren't required to meticulously track every calorie. The medication was combined with general education about healthier eating, not rigid calorie counting.
Data confirms this pattern. A recent study found that people on semaglutide 2.4mg lost an average of 14.1% of their body weight after one year, and those on tirzepatide lost 16.5%, without structured calorie-tracking requirements.
Your Appetite Is Already Being Regulated
This is the fundamental difference.
When you're on a GLP-1 medication, your body is already getting biological signals to eat less. You're not fighting your hunger hormones - the medication is working with them.
For many people, this makes calorie tracking redundant. If you're genuinely not hungry and eating appropriate amounts naturally, what's the point of logging it all?
So Should You Track? It Depends
The evidence suggests there's no one-size-fits-all answer. Let's break down when tracking might help and when it might not.
You Probably Don't Need to Track If:
You're losing weight steadily without it. If you're seeing consistent progress at a pace that feels sustainable (generally 1-2 pounds per week), tracking won't make the medication work better. Don't fix what isn't broken.
You're eating when hungry and stopping when full. If the medication is effectively regulating your appetite and you're making generally nutritious food choices, adding tracking could be unnecessary mental load.
You have a history of disordered eating or obsessive food thoughts. For people with this history, calorie tracking can trigger unhealthy patterns - even with the appetite regulation from GLP-1 medications. The risk outweighs any potential benefit.
The idea fills you with dread. If tracking feels like it would make your life significantly worse, that psychological cost matters. Sustainable weight loss requires an approach you can actually maintain.
You're meeting your protein goals without tracking. More on this in a moment, but if you're naturally eating adequate protein (around 25-40g per meal), that's the most important nutritional metric for GLP-1 users.
Tracking Might Be Helpful If:
You're not losing weight as expected. If you've been on a stable dose for several weeks and aren't seeing progress, tracking for a week or two can reveal patterns. Are you eating more than you realize? Not eating enough? The data can be illuminating.
You're significantly undereating. Some people on GLP-1 medications eat so little they feel fatigued, lose hair, or feel weak. Tracking can help ensure you're actually eating enough- especially enough protein.
You're a data-driven person who finds it motivating, not stressful. Some people genuinely enjoy tracking and find it helps them stay engaged with their health goals. If that's you, and it doesn't trigger anxiety, go for it.
You're trying to dial in specific nutrition goals. If you're working with a healthcare provider on specific protein, fibre, or other targets, tracking can help you hit those marks.
You're in a weight loss plateau. Sometimes tracking reveals sneaky extra calories that have crept back in over time - liquid calories, larger portions, more frequent snacking. A temporary tracking stint can help identify the issue.
A Middle-Ground Approach
You don't have to choose between rigid tracking and complete free-for-all. Many people find success with:
Tracking protein only. Use an app to log just your protein intake, ignoring everything else. This ensures you're protecting muscle mass (more on this next) without the mental load of tracking everything.
Periodic check-ins. Track for one week every month or two, just to make sure you're still on track. Think of it like a periodic audit, not a daily requirement.
Loose awareness without logging. Simply being more mindful of portion sizes and food choices, without the formal tracking. For many GLP-1 users, this is enough.
Photo logging. Some people find taking photos of meals less burdensome than entering data, while still creating accountability.
The Real Nutritional Priority: Protein, Not Calories
Here's what the research on GLP-1 medications has made clear: if you're going to track anything, protein matters far more than total calories.
Why Protein Is Critical on Weight Loss Medications
Studies show that 25-40% of weight lost on semaglutide can come from lean mass (including muscle), and about 26% with tirzepatide. This is actually similar to any weight loss method, but it's still concerning.
Losing muscle has real consequences:
Reduced metabolic rate
Decreased strength and function
Poorer blood sugar control (yes, even on a GLP-1 medication)
Increased risk of frailty, especially in older adults
Recent research found that in people taking semaglutide, eating less protein was linked to greater muscle loss. The study also showed that losing more muscle was associated with less improvement in blood sugar levels - meaning muscle preservation may actually enhance the medication's metabolic benefits.
How Much Protein Do You Need?
Evidence-based recommendations for GLP-1 users:
Minimum: 1.2-1.6 g per kg of body weight per day (roughly 0.5-0.7 g per pound). This is a reasonable target for muscle maintenance during weight loss.
If you're doing resistance training: 1.6-2.2 g per kg (roughly 0.7-1.0 g per pound). The combination of higher protein and strength training is powerful for preserving muscle.
Practical translation: Aim for 25-40 grams of protein per meal. This optimizes muscle protein synthesis better than getting all your protein in one sitting.
The Challenge: GLP-1 Medications Reduce Appetite... Including for Protein
Here's the catch: the same medication that helps you eat less overall can make it harder to eat enough protein.
When you're genuinely not hungry, forcing down a large chicken breast feels impossible. This is where tracking protein specifically can be genuinely useful… not to restrict, but to ensure adequacy.
Strategies that help:
Prioritise protein first at each meal
Use protein shakes when solid food feels like too much
Choose more protein-dense options (Greek yogurt over regular, for example)
Spread protein throughout the day rather than trying to get it all at once
Case studies of people who successfully preserved muscle on GLP-1 medications showed they were eating 1.6-2.3 g per kg of body weight and doing resistance training 3-5 times per week. One person actually gained lean mass while losing significant fat.
What About Resistance Training?
While not strictly about tracking, this is too important not to mention: resistance training may be the single most powerful intervention for maintaining muscle during GLP-1 treatment, potentially more important than hitting exact protein numbers.
You don't need to become a bodybuilder. Research shows benefit from:
2-3 sessions per week
Compound movements (squats, pushes, pulls)
Consistency over intensity
Even bodyweight exercises like modified push-ups and chair squats can provide the mechanical signal your muscles need to maintain mass during weight loss.
The Psychological Factor Nobody Talks About Enough
Calorie tracking isn't just about numbers - it's about your relationship with food.
For some people, tracking provides structure, reduces anxiety, and creates a sense of control. These people often describe it as "freeing" because they know exactly where they stand.
For others, tracking creates obsession, guilt, and a hyperfocus on numbers that crowds out intuitive eating and enjoyment. These people describe it as exhausting and unsustainable.
The research on eating disorders is worth repeating: in people diagnosed with eating disorders, 75% used calorie tracking tools and 73% felt it contributed to their condition.
If tracking makes you:
Anxious or stressed about food
Unable to eat without checking the calories first
Guilty when you "go over" your targets
Obsessively think about numbers all day
...then it's not helping, even if theoretically it "should."
Your mental health is part of your health. A tracking system that damages your relationship with food isn't worth any weight loss benefit.
What Do Healthcare Providers Actually Recommend?
Most evidence-based GLP-1 programs don't require rigid calorie tracking.
Instead, they typically recommend:
General guidance about balanced nutrition
Specific emphasis on adequate protein
Encouragement of fruits, vegetables, and whole foods
Monitoring for undereating (yes, that's a real concern)
Regular check-ins to assess progress
Some programs, like Weight Watchers' GLP-1 program, offer tracking tools for people who want them, but they're focused more on food quality and protein tracking than strict calorie limits.
The clinical trials that demonstrated the effectiveness of these medications didn't require participants to track calories obsessively - they provided general lifestyle education and support.
The Real Question: What Problem Are You Trying to Solve?
Before you decide whether to track, ask yourself: what am I actually trying to achieve?
If your goal is to lose weight faster: Tracking probably won't accelerate weight loss significantly beyond what the medication is already achieving. The GLP-1 medication is doing the heavy lifting.
If your goal is to ensure you're eating enough: Tracking can be helpful, especially for protein. But you might only need to track periodically or track protein specifically.
If your goal is to understand your patterns: A temporary tracking phase (1-2 weeks) can provide insights without becoming a permanent burden.
If your goal is to feel in control: That's valid, but make sure tracking is actually giving you that feeling, not creating more anxiety.
If your goal is muscle preservation: Focus on protein tracking and resistance training, not total calories.
The Bottom Line
The evidence doesn't support mandatory calorie tracking for everyone on GLP-1 medications.
The medications work by regulating appetite at a biological level. For many people, this makes detailed calorie tracking unnecessary - you're already eating less because you're less hungry, not because you're white-knuckling through restriction.
If you're:
Losing weight steadily
Feeling good
Making generally nutritious choices
Meeting your protein needs
...then tracking calories is optional, not required.
If tracking would make you miserable, or if you have a history that makes it risky, or if you simply don't want to do it - you don't have to. The medication works without it.
But there are situations where tracking (especially protein tracking) can be valuable: when progress has stalled, when you're undereating, or when you're data-driven and find it helpful.
The most important numbers to watch aren't your daily calories. They're:
Your protein intake (25-40g per meal)
Your weekly resistance training sessions (2-3 minimum)
Your overall progress and how you feel
If you do choose to track, make it serve you - not the other way around. The moment tracking becomes a source of stress rather than useful information, it's time to step back.
Remember: these medications are achieving remarkable results without requiring people to become full-time accountants of their food intake.
Your energy might be better spent on resistance training, meal planning for adequate protein, and building sustainable habits than on logging every calorie.
The best approach is the one you can sustain long-term while maintaining both your physical and mental health. For some people that includes tracking. For many others, it doesn't.
And both paths can lead to successful, healthy weight loss.
References
Calorie Tracking Effectiveness Research
Painter SL, et al. (2017). The effect of adherence to dietary tracking on weight loss: Using HLM to model weight loss over time. Journal of Diabetes Research, 2017, 6951495. https://pmc.ncbi.nlm.nih.gov/articles/PMC5568610/
Dunn CG, Turner-McGrievy GM. (2019). Dietary self-monitoring through calorie tracking but not through a digital photography app is associated with significant weight loss: The 2SMART pilot study—A 6-month randomized trial. Journal of the Academy of Nutrition and Dietetics, 119(9), 1525-1532. https://www.sciencedirect.com/science/article/abs/pii/S2212267219302667
Patel ML, et al. (2019). Comparing self-monitoring strategies for weight loss in a smartphone app: Randomized controlled trial. JMIR mHealth and uHealth, 7(2), e12209. https://www.sciencedaily.com/releases/2019/02/190228154839.htm
Patel M, et al. (2021). Digital health tracking tools help individuals lose weight. Stanford Medicine News. https://med.stanford.edu/news/all-news/2021/02/digital-health-tracking-tools-help-individuals-lose-weight-study-finds.html
Banerjee P, et al. (2020). Calorie counting smart phone apps: Effectiveness in nutritional awareness, lifestyle modification and weight management among young Indian adults. Journal of Innovation in Health Informatics, 26(4), 262-269. https://journals.sagepub.com/doi/10.1177/1460458219852531
Patient-Centered Outcomes Research Institute (PCORI). (2019). Comparing calorie counting versus MyPlate recommendations for weight loss. https://www.pcori.org/research-results/2013/comparing-calorie-counting-versus-myplate-recommendations-weight-loss
Calorie Tracking and Eating Disorders
Simpson CC, Mazzeo SE. (2017). Calorie counting and fitness tracking technology: Associations with eating disorder symptomatology. Eating Behaviors, 26, 89-92. https://www.sciencedirect.com/science/article/abs/pii/S1471015316303646
Healthline. (2025). Does calorie counting work? A critical look. https://www.healthline.com/nutrition/does-calorie-counting-work
GLP-1 Clinical Trial Data
Wilding JPH, et al. (2021). Once-weekly semaglutide in adults with overweight or obesity (STEP 1). New England Journal of Medicine, 384, 989-1002.
Jastreboff AM, et al. (2022). Tirzepatide once weekly for the treatment of obesity (SURMOUNT-1). New England Journal of Medicine, 387, 205-216.
Jastreboff AM, et al. (2024). Tirzepatide as compared with semaglutide for the treatment of obesity. New England Journal of Medicine, 391, 2159-2170. https://www.nejm.org/doi/full/10.1056/NEJMoa2416394
Lian J, et al. (2025). Real-world weight loss observed with semaglutide and tirzepatide in patients with overweight or obesity and without type 2 diabetes (SHAPE). Advances in Therapy, 42(1), 247-262. https://pmc.ncbi.nlm.nih.gov/articles/PMC12579654/
Samson SL, et al. (2024). Real-world effectiveness of tirzepatide versus semaglutide on HbA1c and weight in patients with type 2 diabetes. Diabetes Therapy, 16(1), 167-183. https://pmc.ncbi.nlm.nih.gov/articles/PMC12579026/
Muscle Loss and Lean Mass Research
Heymsfield SB, et al. (2025). New GLP-1 therapies enhance quality of weight loss by improving muscle preservation (BELIEVE study). American Diabetes Association 85th Scientific Sessions. https://diabetes.org/newsroom/press-releases/new-glp-1-therapies-enhance-quality-weight-loss-improving-muscle-0
Lundgren JR, et al. (2021). Healthy weight loss maintenance with exercise, liraglutide, or both combined. New England Journal of Medicine, 384, 1719-1730.
Neeland IJ, et al. (2024). Changes in lean body mass with glucagon-like peptide-1-based therapies and mitigation strategies. Diabetes, Obesity and Metabolism, 26(9), 3579-3594. https://dom-pubs.onlinelibrary.wiley.com/doi/10.1111/dom.15728
Batsis JA, et al. (2024). Muscle mass and glucagon-like peptide-1 receptor agonists: Adaptive or maladaptive response to weight loss? Circulation, 150, 1948-1962. https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.124.067676
Ida S, et al. (2024). Preservation of lean soft tissue during weight loss induced by GLP-1 and GLP-1/GIP receptor agonists: A case series. Obesity Science & Practice, 10(5), e70012. https://pmc.ncbi.nlm.nih.gov/articles/PMC12536186/
Naimi SS, et al. (2024). The effects of GLP-1 agonists on musculoskeletal health and orthopedic care. Current Reviews in Musculoskeletal Medicine, 17, 433-445. https://pmc.ncbi.nlm.nih.gov/articles/PMC12325148/
Highbar Health. (2025). GLP-1 drugs and muscle loss: What patients need to know. https://www.highbarhealth.com/blog/glp1-drugs-muscle-loss-guide/
Protein Intake and Muscle Preservation
Haines M, et al. (2025). Consuming more protein may protect patients taking anti-obesity drug from muscle loss. Presented at ENDO 2025, Endocrine Society Annual Meeting. https://www.endocrine.org/news-and-advocacy/news-room/endo-annual-meeting/endo-2025-press-releases/haines-press-release
Ivím Health. Lean muscle preservation estimator & protein intake calculator. https://www.ivimhealth.com/lean-body-mass-protein-calculator/
Silva R. (2025). GLP-1 and muscle loss: Semaglutide, tirzepatide & lean mass. Potere Health MD. https://www.poterehealthmd.com/post/glp1-muscle-loss-semaglutide-tirzepatide
Nunes EA, et al. (2022). Systematic review and meta-analysis of protein intake to support muscle mass and function in healthy adults. Journal of Cachexia, Sarcopenia and Muscle, 13(2), 795-810.
GLP-1 Mechanism and General Information
Cleveland Clinic. (2025). GLP-1 agonists: What they are, how they work & side effects. https://my.clevelandclinic.org/health/treatments/13901-glp-1-agonists
Nauck MA, et al. (2024). Glucagon-like receptor-1 agonists for obesity: Weight loss outcomes, tolerability, side effects, and risks. Obesity Pillars, 12, 100228. https://pmc.ncbi.nlm.nih.gov/articles/PMC11404059/
Epic Research. (2024). Tirzepatide and injectable semaglutide correlated with greatest weight loss among GLP-1 medications. https://epicresearch.org/articles/tirzepatide-and-injectable-semaglutide-correlated-with-greatest-weight-loss-among-glp-1-medications
Nuvance Health. (2024). Tirzepatide or semaglutide, weight loss drugs explained. https://www.nuvancehealth.org/health-tips-and-news/weight-loss-drugs-explained
Supportive Programs and Lifestyle Integration
Weight Watchers. GLP-1 weight-loss program. https://www.weightwatchers.com/us/how-it-works/glp-1-program
Intermountain Healthcare. (2024). Your friendly guide to GLP-1 weight loss: What works, what doesn't and what's next. https://intermountainhealthcare.org/blogs/article/your-friendly-guide-to-glp-1-weight-loss-what-works-what-doesnt-and-whats-next